SARS-CoV-2, the virus that causes COVID-19, is thought to spread mainly through direct transmission from person-to-person. However, we are still learning about how it is spread and there are concerns of indirect transmission (person-to-surface-to-person). Because of the anticipated potential for indirect transmission, cleaning and disinfection to reduce risks related to COVID-19 (the illness caused by the SARS-CoV-2 Coronavirus) is a ubiquitous recommendation and a service that has become in high demand. The following is one example recommendation taken from the COVID-19 Industry Guidance prepared by the California Department of Public Health (CDPH) and Cal OSHA. “Perform thorough cleaning on high traffic areas such as break rooms and lunch areas, and areas of ingress and egress including stairways, stairwells, escalators, handrails, and elevator controls. Frequently disinfect commonly used surfaces including doorknobs, toilets, and handwashing facilities. To disinfect, use products that meet EPA’s criteria, the cause of COVID-19, and are appropriate for the surface.”
This summary of cleaning disinfection covers disinfection basics, benefits and limitations of various technologies, includes some SARS-CoV-2 specific information and provides information about the resources that are available. It is not intended to fully cover all the important details about disinfection processes. Aggressive cleaning and surface disinfection are becoming commonplace and even routine in homes, schools, offices and other settings. While some applications are effective, others can be potentially dangerous and knowing which is which may be difficult. Please review the resources listed at the end of this discussion if you want to gain a more in depth understanding of these issues.
What is the Difference Between “Cleaning” and Disinfecting”?
Let’s start with some standard definitions. Per the Centers for Disease Control and Prevention (CDC), cleaning is defined as “the removal of germs, dirt, and impurities from surfaces. It does not kill germs, but by removing them, it lowers their numbers and the risk of spreading infection”. Disinfecting is defined as “using chemicals, for example, EPA-registered disinfectants, to kill germs on surfaces. This process does not necessarily clean dirty surfaces or remove germs, but by killing germs on a surface after cleaning, it can further lower the risk of spreading infection”. Both can be useful and often both are necessary. For example, contamination that could prevent the disinfecting agent from contacting any viruses would need to be removed through cleaning prior to disinfection. As noted above, this process itself can reduce risk. However, the act of cleaning is not without some risk of exposure and therefore it must be done carefully following safe work practices. There is also no escaping the need for frequent, effective hand hygiene during cleaning or when applying a disinfectant. This is true even if the disinfectant used can inactivate the virus which stops it from being infectious.
Disinfectants: A Deep Dive
Disinfectants kill or irreversibly inactivate targeted microorganisms. They must have the proper biocidal or viricidal activity for the targeted pathogen to be effective. They must also come in direct contact with the agent at the proper concentration and for the necessary time. The time element is commonly referred to as contact time. Disinfectants have the potential to cause harm to the person applying them during or after application as these disinfectants are designed to kill or permanently and irreparably damage these pathogens.
Several agencies regulate the use of surface disinfectants. At the federal level examples include the US EPA (EPA), US FDA and OSHA. Both EPA and FDA regulate fumigation, which is a method of application. Fumigation can include the application of sanitizers, sterilizers and disinfectants. OSHA enforces standards to protect workers from occupational hazards. Additionally, state and local public health agencies may have additional rules governing the use of disinfectants.
Below, we’ll answer commonly asked questions about disinfectants and how they relate to SARS-CoV-2.
Q: Can disinfectants kill SARS-CoV-2 on surfaces?
One of the rare instances of “good” news regarding SARS-CoV-2 is that it is an enveloped virus. Enveloped viruses are more easily inactivated by many types of disinfectants than nonenveloped viruses or many pathogenic bacteria. The chart below shows susceptibility of various pathogens.
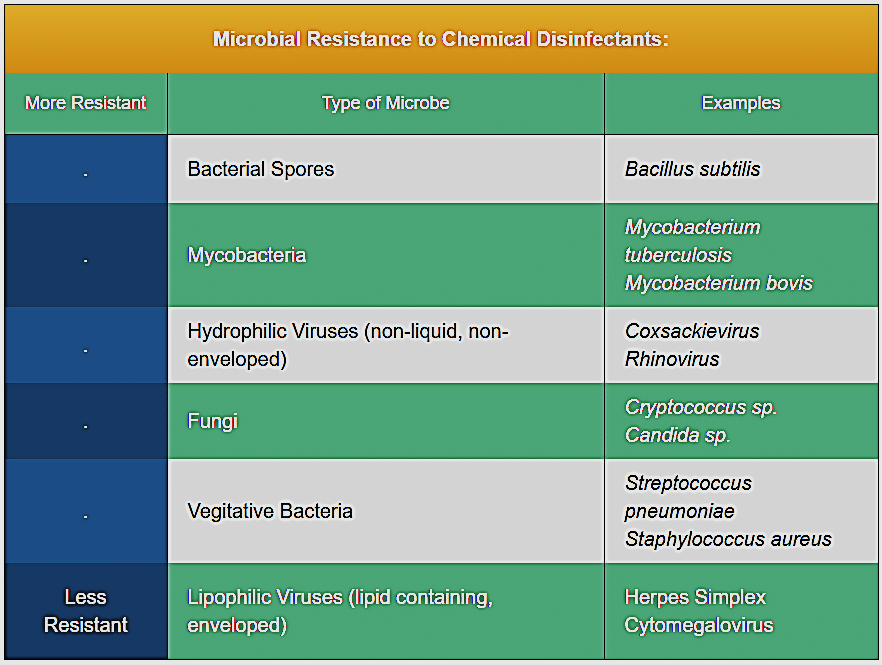
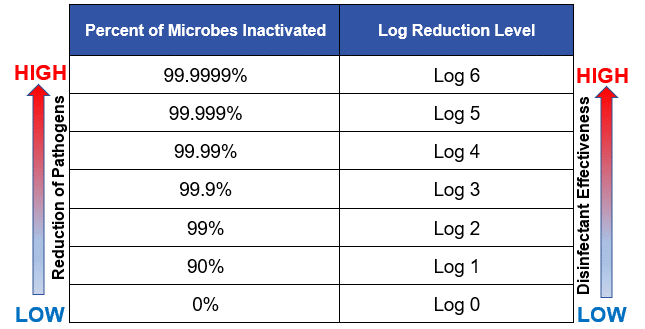
This means that if cleaning and disinfection are done well, the risk of infection from exposures to environmental surfaces where SARS-CoV-2 has been present may be greatly reduced or eliminated. EPA has prepared a list of registered products for use against SARS-CoV-2. This roster, List N, currently includes over 400 products. The EPA registration list provides information for each product listed including but not limited to the active ingredient(s), the product and manufacturer name, the virus(es) for which it is registered, the required contact time, the surface type (non-porous, food contact, porous; Note: very few registered products have a porous surface application claim), use site (healthcare, institutional, residential), and if it has an Emerging Viral Pathogen Claim. For Emerging Viral Pathogens, the EPA looks at how the product performs against viruses that are more difficult to inactivate such as non-enveloped viruses. The package that the manufacturer prepares for EPA registration includes even more details including the methods of application that must be followed. It may also include how much of the viral load is expected to be reduced. This reduction factor is commonly referred to as the log reduction, which is a mathematical term that is used to express the relative number of living microbes that are eliminated by disinfection. When considering disinfectants, higher numbers are preferable as shown in the chart below.
Registered disinfectants are considered pesticides by EPA. The EPA states that “it is a violation of FIFRA to use a registered pesticide in a manner inconsistent with its labeling. Applying products using a different method than what is described in the directions for use on the label could affect the efficacy and safety of the product. For example, if an EPA-registered product’s label specifies that it can only be applied as a liquid using a cloth, sponge or sprayer, then applying it via a fogging device or electrostatic sprayer (which EPA considers a different application method than a conventional sprayer) would be a violation of FIFRA. In addition, applying a product in a way that does not align with its intended use may render the product less effective. For example, a product may have a required contact time (the amount of time a surface must remain wet in order to kill a certain pathogen). If you use an application method that EPA hasn’t evaluated, the surface may not remain wet for long enough, and the product may not be effective.”
Q: What about other disinfectant technologies, such as ultraviolet light or application of gasses or vaporized chemicals, such as hydrogen peroxide?
At this time, the most common applications are chemicals like those discussed above. Ultraviolet Germicidal Irradiation (UVGI) has been well studied and has been used in healthcare to disinfect patient rooms after cleaning to reduce pathogens on surfaces. Systems in place to reduce airborne pathogens in areas above the head of the occupants have been introduced and studied. Upper room UVGI has been studied for the control of airborne pathogens, such as tuberculosis.
One four-month study concluded that Upper-room UVGI devices can reduce bioaerosols, however, there are some important limitations. As with other methods, the disinfectant (in this case ultraviolet light) must contact the pathogen. In order to contact the pathogens, the surfaces must be clean before UV light application and cannot be shadowed from the light. The proper dose concentration is also needed which requires very specific types of UVGI systems. Application of UVGI requires special equipment and training on its proper use, and exposures to UV-C light can be harmful to humans.
Use of vaporized chemicals such as hydrogen peroxide or chlorine dioxide have also been studied and found to be effective disinfectants for viruses., however, the application method is important. Use of a misting application is acceptable if the registration allows for that method, but these methods also require special equipment and training. Using a fogger to create a cloud that wafts through an entire room (referred to as whole room disinfection) is considered use of a fumigant and subject to additional regulations. These application methods present health risks to the people performing the disinfection and possibly to those that come into the room afterwards.
Disinfectants with SARS-CoV-2: The Bottom Line
So, while these technologies are promising, they can be costly, difficult to apply properly and as with other methods, the actions taken after implementation are very important.
The GOOD. When it comes to SARS-CoV-2, this virus is relatively easy to inactivate. We can greatly reduce the risk of indirect transmission through good cleaning and disinfection practices. As noted on the World Health Origination’s COVID-19 website, “The most important thing to know about coronavirus on surfaces is that they can easily be cleaned with common household disinfectants that will kill the virus.” (WHO; April 17, 2020). If we do what we can to limit the spread, we can reduce risk to ourselves and others.
The BAD. Cleaning and disinfecting a space, while essential, may not be enough. The potential to re-contaminate a space remains until the number of new infections has been greatly reduced. At this time, aggressive measures to stop the spread are still needed. This indicates the need for frequent, effective hand hygiene; physical distancing, face coverings and repeated environmental cleaning and disinfection.
The Ugly. Underinformed people may make poor decisions. Many things can go wrong when environmental cleaning and disinfection is not completed properly. We may gain a false sense of security thinking the environment is now completely safe. This may cause some to let their guard down, resulting in exposures to viruses that were not inactivated or performing less effective hand hygiene. Exposures to harmful disinfectants may also result in injury and illness. Improper use may result in violations of laws and regulations designed to protect the public health and the environment and may also cause damage to surfaces. Damage to surfaces can be more than just inconvenient -it can allow those surfaces to more easily harbor contamination and become more difficult to clean in the future.
Ask questions. If someone is proposing a disinfection product that is not on the EPA List N or they cannot produce independent, peer-reviewed studies that support its safe use, seek out more information before you agree to its use.
To become informed, seek out reputable information. Below are several valuable resources that you can use:
- Guidelines for the Selection and Use of Environmental Surface Disinfectants in Healthcare; AIHA 2017
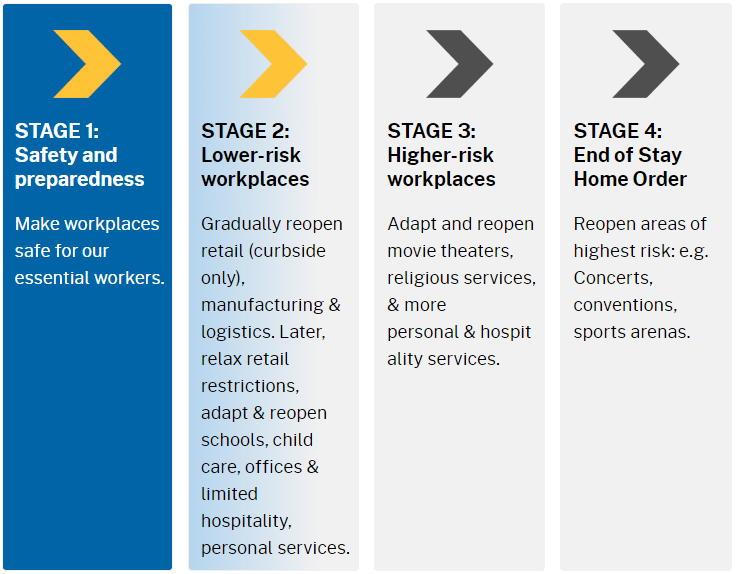
- COVID-19 Industry Guidance; this is hot off the press from CDPH/Cal OSHA with guidance for various businesses and occupancies so they can move from Stage 1 to Stage 2 and beyond.
It is important to always remember that cleaning prior to disinfection may be the most important step. Cleaning can remove contaminants that prevent contact between the pathogen and the disinfectant. Cleaning may also remove the pathogen itself, lowering the total concentration before disinfection even starts. A study conducted by EPA looking at how effectively various cleaners removed a difficult-to-remove contaminant from surfaces concluded that “the effort put into the cleaning may be more important than the choice of cleaner”. Physical labor can be expensive but can also be the most important part of any cleaning and disinfection actions.
Finally, and most importantly, stay vigilant at controlling the things you can control. The chain of person-to-person transmission is broken best by staying away from others if you are sick; washing your hands frequently; maintaining safe physical distance at all possible times; covering our faces in public – especially for coughs and sneezes; and cleaning and disinfecting those surfaces that present risk of indirect transmission.
For assistance, call FACS: (888) 711-9998.